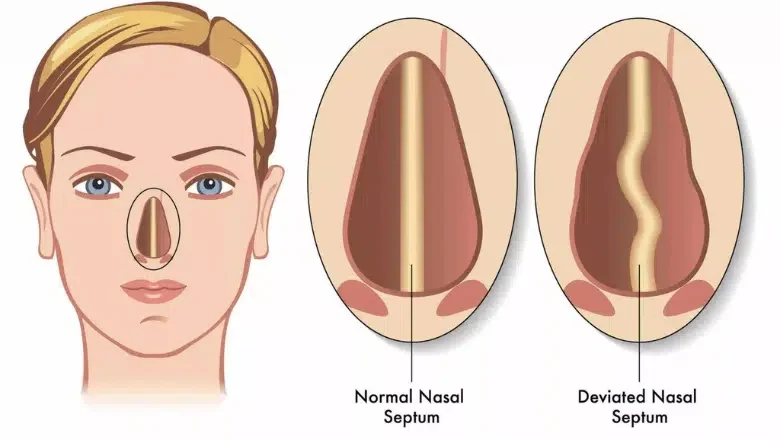
A deviated septum is a condition that affects the structure inside your nose. The septum is the thin wall made of cartilage and bone that separates the two nasal passages. Ideally, this structure should sit in the middle, allowing equal airflow through both nostrils. However, in many people, the septum is not perfectly aligned. Instead, it is shifted or bent to one side, making one nasal passage narrower than the other. This is what surgeons refer to as a deviated septum.
There are several reasons why someone might have a deviated septum. In some cases, it is present from birth due to how the nose developed. For others, it occurs during birth itself, particularly if there is pressure on the baby’s nose during delivery. In many people, the septum becomes deviated over time due to repeated minor injuries. During childhood, it is common to experience small knocks and bumps to the nose, whether from falling, playing sports, or other everyday activities. These minor traumas often go unnoticed at the time, but they can gradually affect the shape of the nasal cartilage. As a result, one side of the nasal passage becomes significantly narrower than the other, leading to persistent breathing difficulties.
Centre for Surgery in London is considered one the leading specialist centres in the UK for for both aesthetic and functional nose surgery.
Recognising the Signs of a Deviated Septum
One of the most common signs of a deviated septum is difficulty breathing through one nostril. Many people experience normal nasal cycles, where the body naturally alternates airflow between nostrils every few hours. However, for someone with a deviated septum, one side is consistently more blocked than the other. This can cause ongoing discomfort, particularly when trying to breathe through the nose during sleep or exercise.
Some people may also experience frequent nasal congestion, a feeling of pressure in the nose, or a tendency to breathe more through the mouth. If these symptoms are persistent, it is advisable to consult an ENT specialist, who can examine the nasal passages and confirm whether a deviated septum is present.
Benefits of Deviated Septum Surgery
One of the most significant advantages of deviated septum surgery is its ability to dramatically improve breathing. If you struggle with persistent nasal obstruction, particularly on one side, a septoplasty can be a life-changing procedure. By straightening the septum, the surgery helps restore balanced airflow through both nostrils, making it easier to breathe, especially during physical activities or while sleeping.
Many people do not realise that the larger side of the nose—the one where the septum has deviated away from—can sometimes feel even more blocked than the smaller side. This happens because of internal nasal structures known as turbinates. These curved, bony structures are responsible for warming, humidifying, and filtering the air you breathe. However, in people with allergies or those living in busy urban environments like London, where air quality may be compromised, the turbinates can become inflamed and swollen. When combined with a deviated septum, this swelling can worsen breathing difficulties, as the turbinate on the larger side expands to compensate for the extra space. This is called compensatory hypertrophy.
If the surgery only corrects the position of the septum without addressing the enlarged turbinate, breathing issues can persist even after the procedure. For this reason, many surgeons perform septoplasty alongside turbinate reduction surgery. This dual approach not only straightens the septum but also reduces the size of the swollen turbinates, ensuring that airflow is properly restored on both sides of the nose.
RELATED: Pros and Cons of Turbinate Reduction with Septoplasty
Another key benefit of septoplasty is that it can lead to better sleep quality. Many people with a deviated septum experience snoring, restless sleep, or even sleep apnoea due to poor nasal airflow. Surgery can significantly enhance sleep patterns by improving nasal breathing, leaving patients feeling more rested and energised.
In addition, septoplasty may also help reduce chronic sinus infections. When one side of the nose is consistently blocked, mucus can build up, creating an environment for bacteria to grow. Restoring normal airflow and drainage can lower the risk of recurrent sinusitis and related symptoms, such as facial pressure, headaches, and postnasal drip.
While septoplasty does not change the external appearance of the nose, many patients report an overall improvement in quality of life after the procedure. Breathing freely through both nostrils can make a noticeable difference in everyday activities, from exercising to simply feeling more comfortable throughout the day.
Potential Drawbacks of Deviated Septum Surgery
While septoplasty offers significant benefits, there are also some drawbacks and limitations to consider before undergoing surgery. One of the key challenges is that nasal obstruction is highly subjective. What one person perceives as severe breathing difficulty might not feel as problematic to someone else with a similar degree of septal deviation. There are multiple factors that contribute to how we breathe, including allergies, turbinate size, nasal inflammation, and environmental conditions. Because of these variables, the extent of deviation in the septum does not always directly correlate with the level of nasal obstruction experienced by the patient.
From a medical and scientific standpoint, this makes it difficult to measure exactly how much improvement a patient will achieve after surgery. Unlike other surgical procedures where outcomes can be more precisely predicted, septoplasty results can vary depending on other nasal structures, such as the turbinates, and external factors like air quality and sinus health.
Correcting it surgically for most people with a significantly deviated septum should lead to noticeable breathing improvements. However, it is important to understand that septoplasty does not always provide 100% relief. In some cases, patients may still experience some degree of nasal congestion or obstruction after surgery, particularly if other underlying conditions—such as allergies or chronic sinus inflammation—contribute to their breathing difficulties. While the surgery often brings substantial improvement, it is not guaranteed to completely eliminate all breathing issues.
RELATED: Can Nose Surgery Treat Nose Allergies?
Another potential drawback is the recovery process. After surgery, patients typically experience swelling, congestion, and mild discomfort for several weeks. During this period, breathing through the nose can feel restricted, and it may take time before the full benefits of the procedure are noticeable. While complications are rare, there is a small risk of infection, bleeding, or scar tissue formation, which could affect the outcome.
Additionally, septoplasty does not alter the external appearance of the nose. If a patient has a visibly crooked nose due to a deviated septum and wants to improve both function and aesthetics, they may need to consider a septorhinoplasty, which combines septoplasty with cosmetic nasal reshaping.
RELATED: Can Rhinoplasty and Septoplasty Be Done Together?
How Severe Does a Deviated Septum Need to Be for Surgery?
The decision to undergo septoplasty depends largely on the individual’s experience of nasal obstruction rather than just the degree of deviation. Everyone perceives breathing difficulties differently, which means that even a minor deviation of just a millimetre or two can feel significantly obstructive for some people. In contrast, others may have a severely deviated septum yet only feel a moderate improvement after surgery. This variation occurs because nasal airflow is influenced by multiple factors, not just the position of the septum.
One important factor that can contribute to persistent nasal obstruction is the internal nasal valve, which is the narrowest part of the nasal airway. This valve is located at the junction between the nasal bone and the cartilage, and its natural angle should be between 10 to 15 degrees. If this angle is slightly narrower, it can create significant breathing difficulties. In some cases, people who have already had septoplasty and turbinate surgery may still experience obstruction due to narrowing of the nasal valve.
For patients with internal valve collapse, additional surgical techniques such as cartilage grafting may be required. This involves taking cartilage from another part of the nose and strategically placing it to widen the internal nasal valve. This can help optimise airflow and resolve residual breathing difficulties that septoplasty alone may not fully address.
Since nasal obstruction is subjective, there is no single threshold for when surgery is necessary. However, a general guideline is that if one side of your nose feels consistently blocked, making it difficult to breathe through, and if you can visibly see a deviated septum inside the nostril, then septoplasty is likely to provide some level of improvement.