Many individuals considering the removal of breast implants often inquire about the various choices available after surgery. Understanding these options is crucial for making an informed decision that aligns with one’s aesthetic goals and health requirements.
Breast implant removal surgery primarily focuses on the safe extraction of implants from the patient’s body. Over time, breast implants, much like any other medical device, can degrade. Typically, implants have an effective lifespan of about 10 to 15 years, after which they may need to be replaced or removed entirely depending on the patient’s preference and health considerations.
One fundamental option is the complete removal of the breast implants without replacement. This choice might appeal to those who wish to revert to their natural breast size or who no longer wish to maintain implants.
Another surgical technique involves the removal of the capsule surrounding the breast implant. This can be done in two ways: either removing the entire capsule through an en-bloc resection or removing only a part of it. This decision often depends on the specific medical circumstances, such as the presence of scar tissue or complications like implant rupture or leakage.
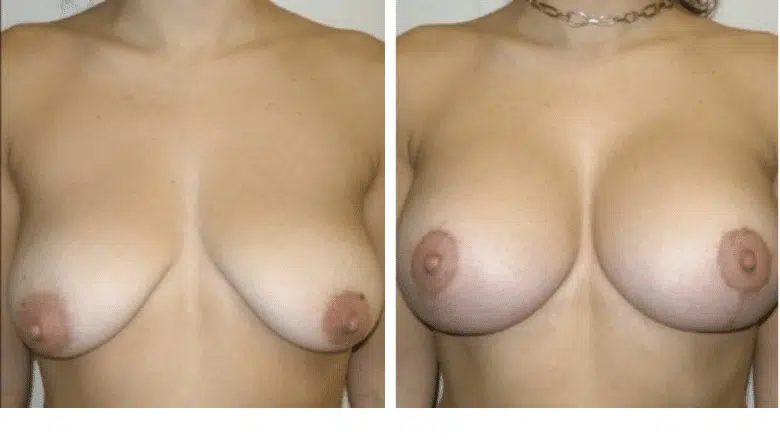
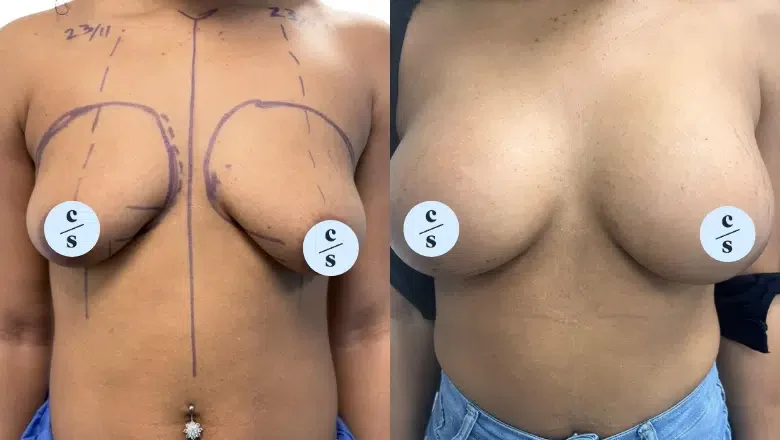
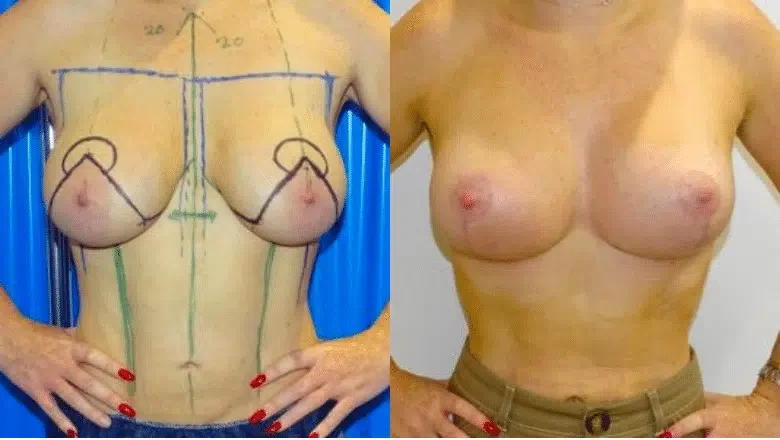
Following the removal of implants, some patients may opt for additional procedures to enhance the appearance of their natural breasts. A common follow-up procedure is a breast lift, or mastopexy, which helps to raise and firm the breasts. Alternatively, breast reduction or fat grafting can also be considered to improve the breast contour and volume post-implant removal.
Life events such as pregnancy can influence the decision to remove breast implants. It is not uncommon for mothers and older patients to choose implant removal as they seek comfort with their natural body shape, having felt that the implants have served their purpose.
Reasons for Replacing or Removing Implants
Breast implants may need to be replaced or removed for several reasons:
Botched Implants
Occasionally, implants do not turn out as expected. This can be due to the surgical technique used or the type of implant selected. Notably, there have been instances where surgeries conducted by less experienced surgeons, particularly from regions with less stringent medical standards such as some areas in Turkey, have led to unsatisfactory outcomes. These surgeons might lack the necessary regard for meticulous surgical technique and postoperative care, leading to increased complications.
Complications
Various complications might prompt the need to replace or remove implants. These include but are not limited to:
-
- Capsular contracture – the formation of tight scar tissue around the implant
-
Implant malposition, which can manifest as:
- High malposition – implants positioned too high on the chest
- Low malposition – implants that have settled too low
- Lateral malposition – implants that have shifted towards the armpits
- Symmastia – implants that create an unnatural connection across the midline, resembling a unibreast
- Implant rupture – when the implant breaks down
- Implant rippling – visible wrinkles or ripples in the implant surface
Concerns with Textured Implants
Textured breast implants, often chosen for their ability to minimise movement within the surgical pocket, have come under scrutiny. These implants, typically tear-drop shaped, are designed to adhere to the body’s tissue, reducing shifting and maintaining position. However, they have been linked to specific challenges:
Aesthetic Concerns
Any rotation or movement of a textured implant can lead to aesthetic deformities due to their shape.
Health Risks
There is a notable association between textured implants and an increased risk of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). This rare cancer of the immune system is not a form of breast cancer but rather a malignancy that can develop from the chronic inflammation caused by the implants. Recent studies, including data from the UK implant registry, suggest that the risk of developing BIA-ALCL can be as high as one in a thousand, which is significant when considering the large number of implant procedures performed.
RELATED: Does Breast Implant Texture Affect the Risk of Complications?
Options and Procedures for Capsule Removal During Breast Implant Removal
When undergoing breast implant removal, patients are presented with several procedural choices regarding the handling of the capsule, the layer of scar tissue that naturally forms around the implant. Understanding these options is crucial for anyone considering or undergoing implant removal.
What is a Capsule in Breast Implant Surgery?
A capsule is the fibrous scar tissue that the body forms around any foreign object, including breast implants. This biological response is a protective mechanism, encapsulating the implant within a defined tissue boundary.
Options for Capsule Management During Implant Removal:
Implant Removal Only
The simplest option involves removing just the breast implants, leaving the capsule intact within the breast. This approach might be suitable if the capsule is thin, healthy, and not causing any discomfort or complications.
Partial Capsulectomy
This procedure involves the removal of the breast implants along with portions of the capsule. A partial capsulectomy is typically performed to address specific issues like capsular contracture, where parts of the capsule have thickened and hardened, causing discomfort or distorting the breast’s appearance. Removed sections can also be sent for pathological evaluation to assess any signs of disease or abnormalities.
RELATED: En Bloc vs Partial Capsulectomy for Breast Implant Removal
Total Capsulectomy
Also known as a complete capsulectomy, this involves the removal of the entire capsule in addition to the implants. The capsule may be removed in one piece or in multiple sections, depending on the circumstances of the surgery and the integrity of the tissue. A total capsulectomy is often recommended if there is concern about the condition of the capsule, such as calcification, thickening, or association with implant rupture.
En Bloc Capsulectomy
A more specific and meticulous version of a total capsulectomy is the En Bloc capsulectomy. This technique ensures that the capsule and implant are removed together as a single unit without opening the capsule. The term “En Bloc”, borrowed from cancer surgery terminology, implies that all potentially affected tissues, including the capsule and implant, are removed in their entirety to minimise the risk of contamination to the surrounding tissues. This method is particularly demanded by patients for its thoroughness and the theoretical reduction in the risk of leakage or spread of any silicone material or other contents from within the capsule.
RELATED: En Bloc Technique For Breast Implant Removal
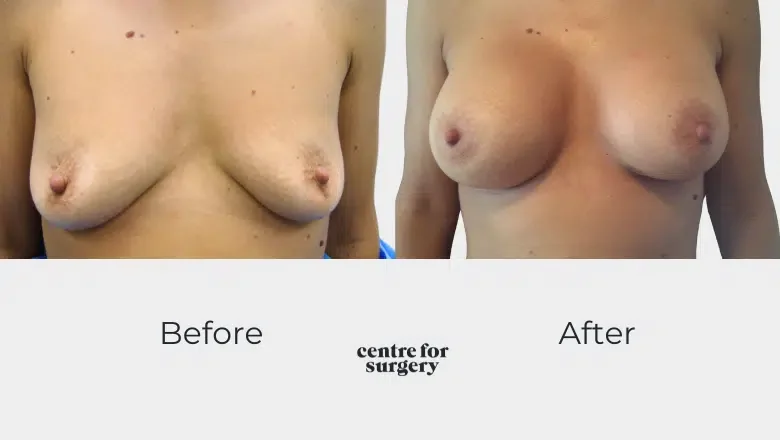
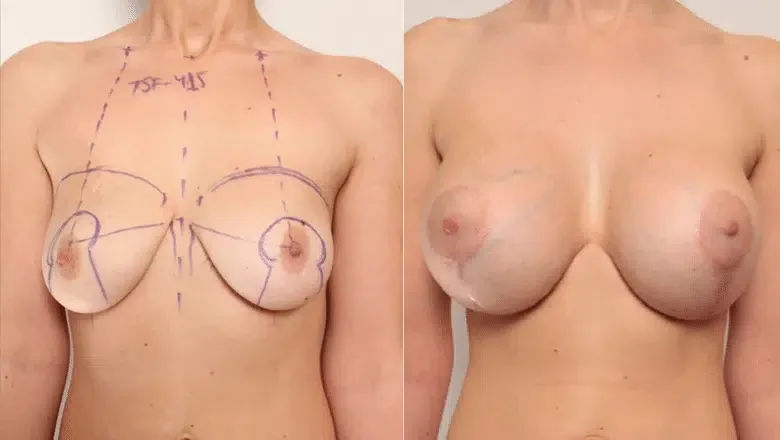
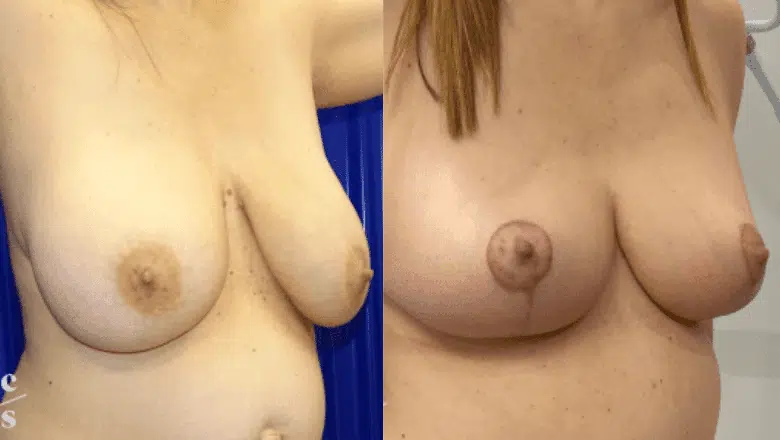
Considering a Breast Lift (Mastopexy) or Reduction After Implant Removal
For many patients, the removal of breast implants presents an opportunity to reassess and potentially enhance their natural breast contour. A common follow-up procedure to implant removal is a breast lift, also known as mastopexy, or a breast reduction. These procedures are designed to improve the shape and position of the breasts following the removal of implants.
Timing of Breast Lift After Implant Removal:
Our surgeons typically advise patients to consider a waiting period before undergoing a breast lift after implant removal. This recommendation is based on several technical and healing considerations:
Technical Complexity
Performing a breast lift immediately after implant removal can be technically challenging. This complexity arises because the surgeon must adjust to the original size and shape of the breast tissue, which might have been altered due to the presence of implants. Waiting allows the breast tissue to settle into a more stable position, making the lift procedure potentially more straightforward and effective.
RELATED: Breast Implant Removal & Breast Lift
Healing and Recovery
Allowing a period of recovery after implant removal gives the breast tissue time to heal and contract. This waiting period, typically around one year, helps ensure that any swelling has subsided and the breast tissue has stabilised, providing a clearer foundation for any further corrective surgery.
Physical and Emotional Readiness
The gap between procedures also gives patients time to recover physically and emotionally from the initial surgery. Deciding to undergo a breast lift is significant, and patients benefit from having time to consider their options and feel ready for another procedure.
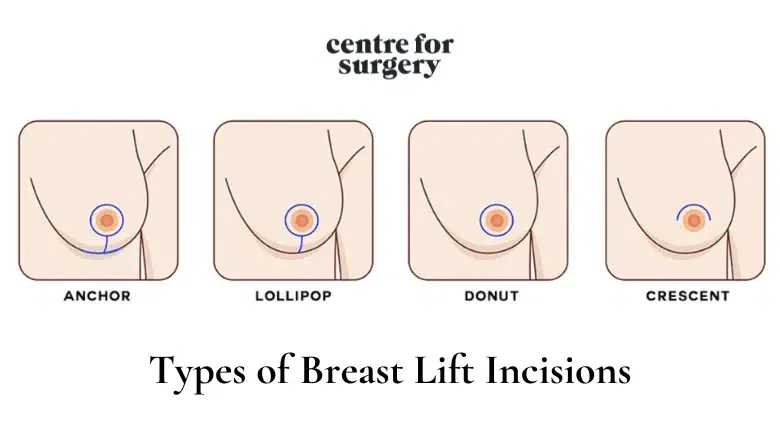
Incision Choices for Breast Lift (Mastopexy)
When undergoing a breast lift, also known as mastopexy, choosing the right type of incision is crucial to achieving the desired aesthetic results while addressing individual anatomical needs. The choice of incision depends largely on the extent of the lift required, the patient’s skin quality, and the presence of any previous scars. Here we explore the common incision techniques used in breast lift surgeries: the circumareolar incision and the inverted-T incision.
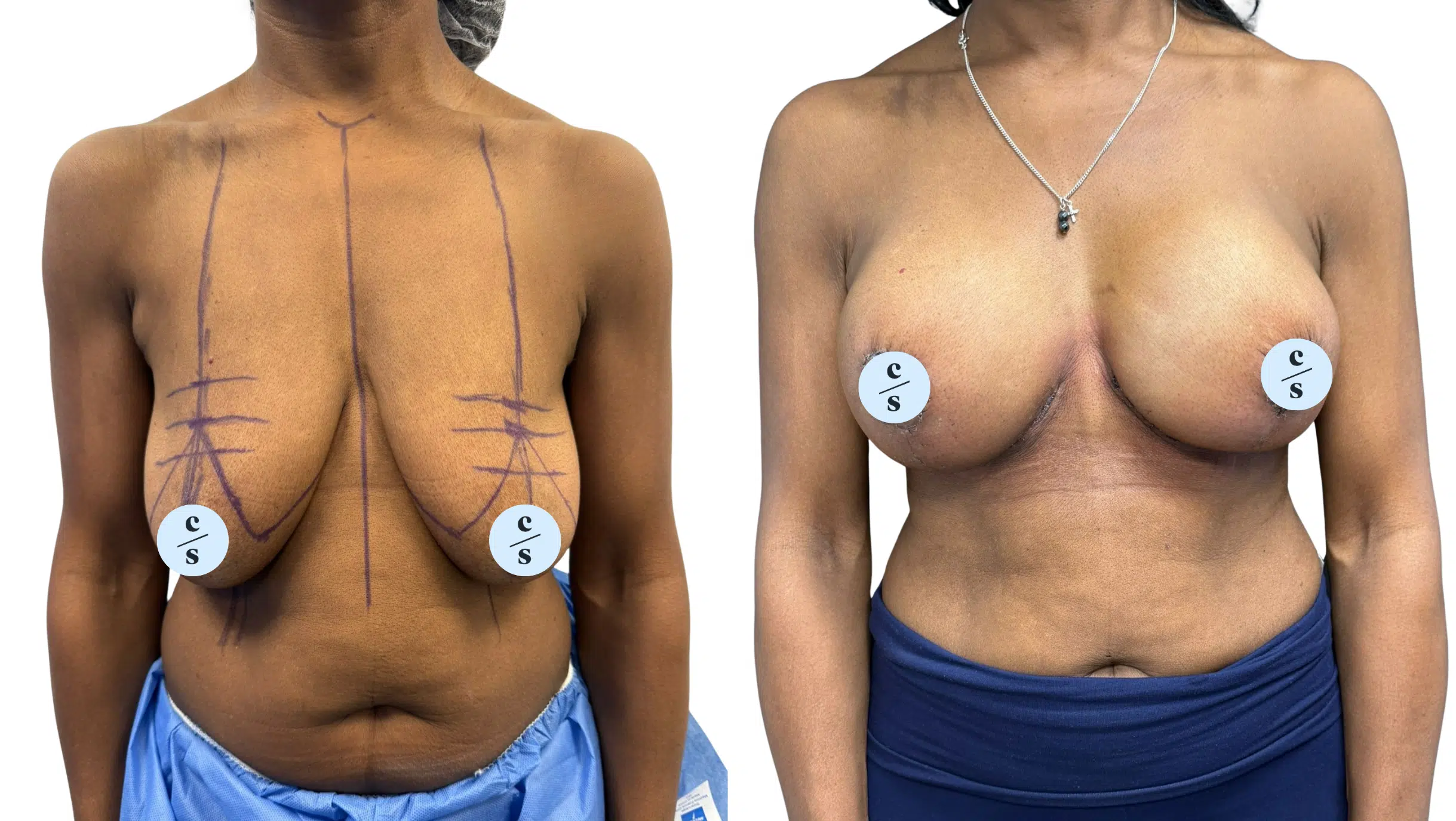
Inverted-T Incision
The inverted-T incision may be recommended for patients with more significant sagging, poor skin elasticity, or those with previous inframammary incisions. This technique is more comprehensive and allows for considerable skin removal and extensive breast reshaping. The incision comprises three parts: around the areola, vertically down from the bottom to the breast crease, and horizontally along the breast crease, forming a shape akin to an inverted “T” or an anchor. This type of incision is ideal for women with heavier breasts and significant breast descent, as it enables the removal of excess tissue and the repositioning of the remaining tissue to a more aesthetically pleasing, elevated position.
The inverted-T incision also allows for the repositioning of descended nipples, enhancing the overall breast contour and symmetry. Although this method results in more visible scarring compared to the circumareolar approach, it offers greater correction and is often necessary for achieving optimal results in cases of severe sagging.
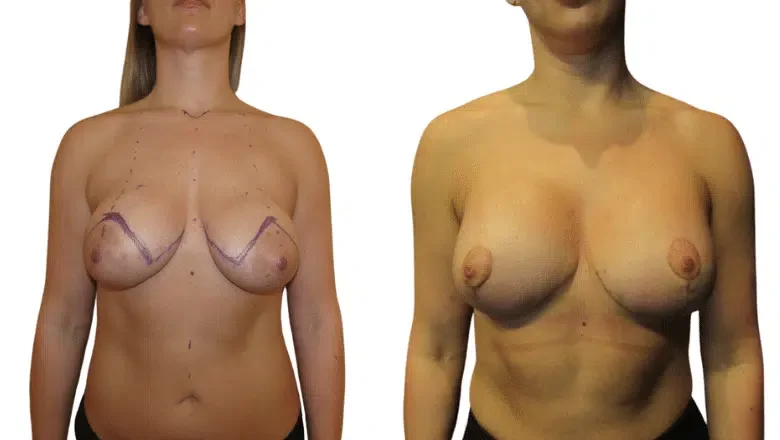
Circumareolar Incision
The circumareolar incision technique, also known as a doughnut breast lift, is often selected for patients who require a mild lift. This approach involves making an incision around the areola. The primary advantage of this method is its subtlety and the minimal scarring it leaves, as the incision blends naturally with the edge of the areola. During this procedure, the breast tissue is lifted, and sutures are strategically placed higher up to subtly elevate the breast’s position. This technique is suitable for those who have had previous breast surgeries where the incision was made around the areola, allowing the same incision site to be used for both implant removal and the lift. This option is less invasive and can effectively enhance the breast’s appearance with minimal additional scarring.
Immediate vs. Delayed Mastopexy
While waiting is generally recommended, some patients may choose to have a breast lift immediately following implant removal. Some patients may prefer to complete their surgical journey as soon as possible for personal or emotional reasons.If the surgeon assesses that the patient’s breast tissue condition and overall health are conducive to immediate lifting, this can be a viable option.
Having a breast lift at the same time as implant removal involves certain risks, such as increased complication rates due to operating on tissue that is still healing from recent surgery. Complications might include issues with wound healing, infections, or suboptimal aesthetic outcomes due to changes in tissue elasticity and shape post-implant removal.
Fat Grafting After Breast Implant Removal
Fat grafting, also known as autologous fat transfer, is a procedure gaining popularity among patients looking to naturally enhance breast volume after removing breast implants. This technique involves augmenting the breasts with the patient’s own fat, harvested from other parts of the body.
The Fat Grafting Procedure
The process starts with liposuction, where fat is removed from areas with excess deposits, such as the abdomen, hips, or back. This step not only provides the material needed for breast augmentation but also improves the contour of the areas from which the fat is taken. Once harvested, the fat is then purified and prepared for injection into the breast area. This method uses the patient’s tissue, reducing the likelihood of allergic reactions and rejection.
Benefits of Fat Grafting
Fat grafting offers a more natural alternative to synthetic implants and generally results in a subtle enhancement. It is less likely to affect the functionality of the breast, including milk ducts and nerves, due to the minimally invasive nature of the injections compared to surgical implant placement. Additionally, the procedure benefits both the breasts and the donor site areas, slimming down the latter while enhancing the former.
Limitations and Considerations
While providing a natural form of enhancement, fat grafting does not achieve the same dramatic increase in size as traditional breast implants. Patients need to manage their expectations about the results. The procedure’s success heavily depends on the availability of sufficient donor fat. Therefore, patients need to discuss with their surgeon whether their body composition makes them a good candidate for fat grafting.
RELATED: Is Fat Grafting to the Breasts Worth It?
Considering Implant Removal After Pregnancy
Pregnancy can significantly change a woman’s body, including her breasts. Women who have breast implants and become pregnant may have concerns about how these implants could affect breastfeeding and the long-term appearance of their breasts.
Breastfeeding with Implants
Generally, breast implants do not interfere with a woman’s ability to breastfeed. The location of the implants plays a crucial role in this. Implants placed under the muscle (subpectoral) or in a dual-plane position are less likely to affect the milk ducts and nerves essential for breastfeeding. Therefore, women with these types of implant placements usually don’t experience difficulties related to breastfeeding.
RELATED: Can You Breastfeed with Implants?
Changes in Breast Size and Shape
During pregnancy, the breasts typically enlarge due to hormonal changes, milk production, and overall weight gain. After childbirth and throughout breastfeeding, the size of the breasts can fluctuate further. Once breastfeeding is completed, the breasts often lose volume and may sag, which can lead to significant changes in their appearance compared to pre-pregnancy. These transformations might make some women reconsider the need or desire for their breast implants.
Breast Appearance after Pregnancy
After pregnancy and breastfeeding, many women notice that their breasts have not only changed in size but have also lost some of their previous firmness or shape. This can result in breasts appearing ‘deflated’ or sagging. It’s common at this stage for women to consider additional cosmetic procedures to restore the appearance of their breasts. A breast lift (mastopexy) is frequently chosen to elevate and reshape the breasts after the significant changes induced by pregnancy and breastfeeding.
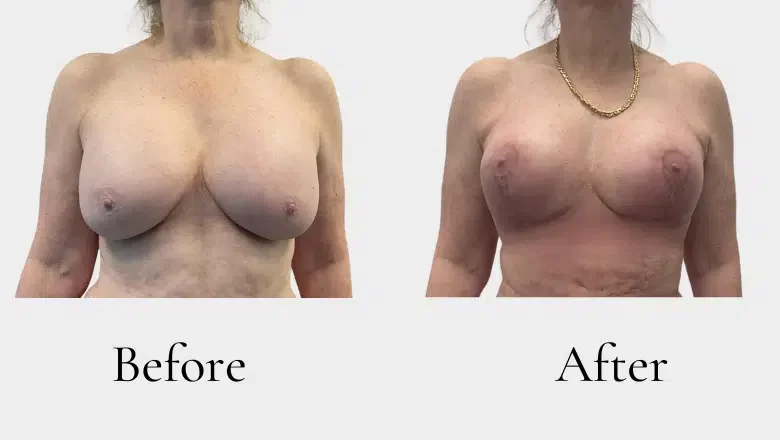
Removing Implants Later in Life
As individuals age, their priorities and health concerns often shift, influencing decisions regarding breast implants. Over time, implants—like any medical device—can wear and potentially require replacement. Traditionally, it’s recommended that breast implants be replaced or reassessed every 10 to 15 years. However, as patients grow older, many opt to remove their implants permanently rather than replace them.
Reasons for Removing Implants in Older Patients
Several factors contribute to the decision among older patients to remove their breast implants. Life events such as becoming a mother or changes in financial status can alter one’s perspective on the necessity of implants. What once seemed essential may no longer hold the same importance. With age, the risks associated with surgery and anaesthesia can become more significant, leading older adults to prefer avoiding additional surgeries, particularly if the implants are not causing discomfort or health issues. As people age, their comfort with their natural body may increase, diminishing the desire for enhanced body features through implants. Recovery times tend to lengthen with age due to slower healing processes, making the prospect of undergoing implant replacement surgeries less appealing.
The Importance of Personalised Approaches in Breast Surgery
When it comes to surgical procedures, particularly those involving breast augmentation, lifts (mastopexy), or implant removal, each individual’s body is unique. This uniqueness demands personalised surgical plans to ensure the best outcomes and highest satisfaction for each patient.
Individual Differences in Body and Breast Anatomy
Each person’s body and breasts differ, including size, shape, tissue density, and how they might react to surgical procedures. These variations significantly influence the type of surgery that may be most effective or appropriate. What works well for one person may not be suitable for another, making personalised treatment plans essential.
Tailoring Procedures to Individual Needs
A skilled plastic surgeon must evaluate each patient’s specific physical characteristics and personal goals to tailor the surgical approach accordingly. This bespoke planning is crucial for achieving the desired aesthetic outcome, minimising risks, and ensuring a smooth recovery.
The Role of Patient-Surgeon Communication
Effective communication between the patient and surgeon is vital. Patients should feel comfortable discussing their expectations, concerns, and any questions they have about the procedure. Patients should fully understand all aspects of the proposed surgery, including the risks, benefits, and any alternatives. This knowledge allows them to make an informed decision about whether to proceed with surgery.
Questions to Consider Before Surgery
For those considering implant removal or any breast-related surgery, here are a few questions to discuss with your surgeon:
- How will my body type and breast anatomy affect the surgery?
- What are the expected outcomes based on my specific case?
- What are the potential risks and how are they managed?
- What can I expect during the recovery process?
Why Choose Centre for Surgery: Expertise, Care, and Comprehensive Support
Centre for Surgery is a specialist centre for those seeking expert and compassionate care in breast plastic surgery. Located in the heart of London, our clinic combines cutting-edge techniques with a deep commitment to patient safety and satisfaction.
Dedicated and Experienced Specialists
Our team of surgeons is highly trained and specialises in a range of cosmetic procedures, ensuring that you receive the most advanced and appropriate treatment for your needs. Our surgeons are dedicated to providing personalised care and achieving the best outcomes for each patient.
Patient-Centred Care
We believe that each patient’s journey is unique, and we are committed to supporting you from consultation through to recovery. Our clinic provides a comfortable and confidential environment where all your concerns can be addressed with sensitivity and discretion.
State-of-the-Art Facilities
Located at 95-97 Baker Street, our clinic is equipped with the latest in medical technology, which allows us to perform even the most complex surgeries with precision. The Baker Street clinic not only offers a central and accessible location but also ensures that your treatment is conducted in a safe and welcoming setting.
Patient Testimonials
Hear from our patients about their experiences at Centre for Surgery:
- Sarah from London: “I had a breast augmentation at Centre for Surgery last year, and I couldn’t be happier with the results. The staff were incredibly supportive, and my surgeon was both skilled and kind. The whole process was seamless, and the care I received was outstanding.”
- Kate from Manchester: “After consulting with several clinics, I chose Centre for Surgery for my rhinoplasty. It was the best decision I could have made. The attention to detail and expertise of the team were evident from the first consultation through to my last follow-up appointment.”
- Emma from Bristol: “Choosing Centre for Surgery for my liposuction was a life-changing decision. The results have been fantastic, and the care and advice I received from everyone at the clinic were beyond what I had hoped for.”
Comprehensive Financial Options
Understanding the financial aspect of surgery is crucial, which is why we offer a range of finance options, including 0% APR with Chrysalis Finance. For more details on how to manage the cost of your procedure, visit our Finance Options page.
More Information
For more insights about our services and to read about various topics in cosmetic surgery, visit our Plastic Surgery Blog. Additionally, you can find answers to common questions on our Clinic FAQs page.
Schedule a Consultation
If you are considering plastic surgery, we invite you to schedule a consultation to discuss your options and how we can help you achieve your aesthetic goals. You can reach us at 0207 993 4849 or by email at contact@centreforsurgery.com. Visit our About Us page to learn more about our clinic and what makes us the right choice for your surgical needs.