What are varicose veins?
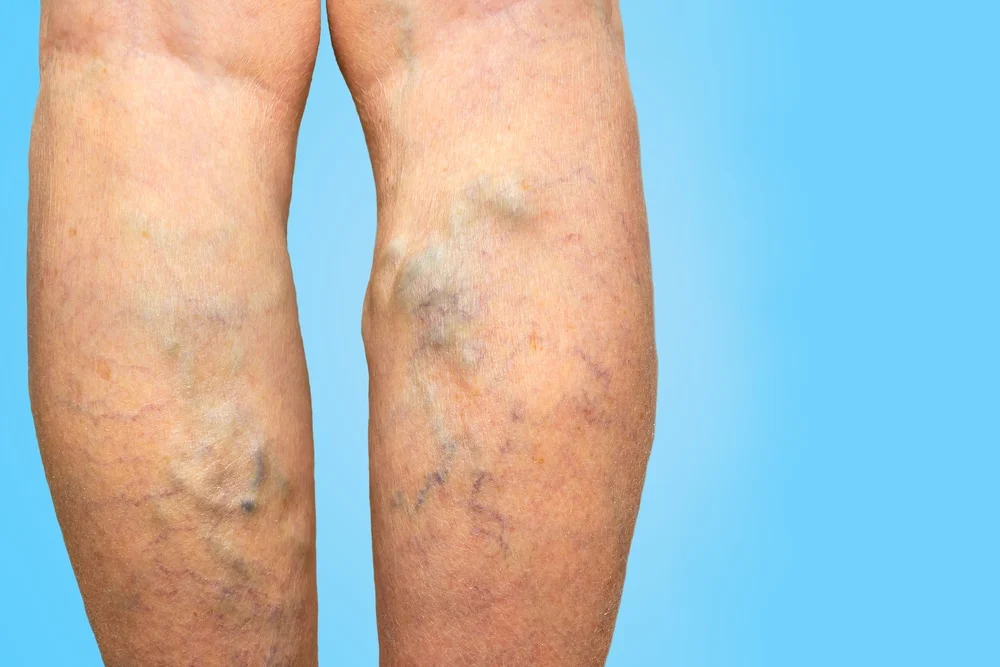
Varicose veins are prominent bulging veins most commonly found on the legs and progressively enlarge over time. The presence of varicose veins usually signifies an underlying defect in valve function in the deeper veins of the leg, which also supply blood to the prominent and visible varicose veins. Thread veins, also known as spider veins are different from varicose veins in that they are much smaller veins often visible below the skin and have a spidery and red-purple colouration.
RELATED: What are varicose veins?
Causes of varicose veins
Varicose veins develop when a valve function defect occurs in the leg’s deep veins that ordinarily propel blood from the peripheries to the heart. These valves are found in all normal veins and function to ensure that blood flows in only one direction. In the case of the leg, the blood only flows upwards from the foot back to the heart. With a failure in the function of these valves, it is possible to develop retrograde blood flow in the opposite direction to the normal path of blood flow. This causes excess venous blood to pool in the veins of the leg and this clinically manifests as a swelling and visible enlargement of the superficial leg veins. The dysfunction of the valves is also known as venous insufficiency and can give rise to a number of clinical presentations.
One of the most common presentations of venous insufficiency is the development of thread veins or spider veins of the leg, which are generally accepted to be only a cosmetic nuisance and not associated with any functional disturbance. In a small number of cases, thread veins can be associated with mild discomfort or aching of the leg. It is also possible to develop a slightly flatter and wider type of leg vein which has a blue colouration and is known as reticular veins or flat feeding vessels.
The most severe form of valve dysfunction in the veins leads to the development of varicose veins. In those aged over 65, a small proportion of patients with varicose veins may go on to develop overlying skin changes and the development of venous ulceration.
All types of prominent leg veins are due to a fundamental build-up of pressure in thin-walled veins which, unlike arteries, are not designed to withstand these high venous pressures.
The causes of venous insufficiency include:
- Obstruction to the deep veins (such as DVT)
- Failure of the calf muscle pump
- Valve dysfunction or failure (most common)
The most common cause of obstruction to the deeper veins is the development of DVT. DVT has several causes, including recent surgery, use of the oral contraceptive pill and certain medical conditions such as cancer. The development of calf muscle failure is related to the underlying weakness of the calf muscles, which can be either present from birth or develop in later life. Permanent calf muscle weakness can also cause valve dysfunction. The most common cause of Venus insufficiency and the development of varicose veins is valve dysfunction, which most commonly arises from genetic defects in the structure of the valve, hormonal changes, traumatic injury, previous DVT or weakness of the calf musculature.
After a valve has stopped working correctly, it does not return back to normal, and this allows the flow of blood to occur in a reverse direction, also known as reflux. This is the wrong direction of blood flow, which should be towards the heart and not away from it. This backflow of blood leads to stretching and enlargement of the vein, followed by a cascade of valve failure extending throughout the entire vein. The end result is invariably the development of varicose veins. Unfortunately, the main underlying reason for the development of varicose veins is related to hereditary factors, which, of course, nothing can be done to change one’s genetic make-up.
The accurate diagnosis and treatment of vein reflux are fundamental to the successful management of venous insufficiency-related conditions, including thread veins, reticular veins, varicose veins and venous ulceration.
Varicose vein clinical features
Varicose veins are responsible for the development of a number of clinical symptoms and signs in the legs. The most common complaints reported by patients include aching, crampiness, itchiness, swelling, leg fatigue and the development of skin changes. In some cases, varicose veins can bleed when subjected to even a trivial injury, especially in older patients. The increase in vein pressure results in the development of skin discolouration, and in the most advanced cases, venous ulceration can develop. Venous ulcers can take a long time to improve without timely treatment. Many patients often endure symptoms of varicose veins not being keen on invasive surgery and not knowing that effective minimally invasive treatments exist. Only after EVLA treatment are patients amazed at the amazing improvement and how they lived for so long with the discomfort of varicose veins.
Our expert practitioners give 3 reasons why they would always recommend seeking treatment for varicose veins, as they can lead to medical complications if left untreated:
- Varicose veins are unsightly. Varicose veins are often more than just a cosmetic nuisance and can significantly impact people’s mental health and well-being. Many people will avoid wearing clothes which expose their legs in public. This has serious impacts on recreational activities and playing sports and even has a personal impact with many patients not displaying their legs to their partner. It can also have professional implications for those who work in the entertainment industry.
- Varicose veins can cause discomfort. Symptoms caused by the presence of venous reflux give rise to the increase in venous pressure and not the actual varicose veins themselves. The most common symptoms include aching, itchiness, leg fatigue and restlessness of the legs. These clinical features can be effectively alleviated with vein treatment.
- Varicose veins can result in damage to the skin and the development of venous ulceration. These medical complications only occur in a minority of untreated cases. Most patients with varicose veins do not go on to develop venous ulcers. However, most venous ulcers patients often have coexisting varicose veins, which both developed in response to increased pressure in the deep veins. Effective treatment of varicose veins leads to a reduction of vein pressure and a much lower likelihood of developing leg ulcers.
Is it possible to have symptoms from varicose veins but for them not to be visible?
In a small number of cases, patients may develop symptoms typically linked with the formation of varicose veins due to valve dysfunction but with no obvious features of varicose veins.
Diagnosis of varicose veins
Colour duplex ultrasound is the gold standard diagnostic technique for precise diagnosis of the underlying cause of prominent leg veins including both thread veins and varicose veins. There is no other effective way to assess the condition of the deep veins to then allow the selection of the correct treatment. Our practitioners have years of experience in carrying out comprehensive and detailed colour duplex scans in patients suffering from all types of leg veins.
Should I see my GP for the diagnosis of varicose veins?
Most varicose veins are obvious on examination and are easily diagnosed on the basis of how they look. This leads many patients to decide not to consult with their GP as they know what they are already. Wherever you have assessment and treatment for leg veins, it is still important to keep your GP informed for continuity of care.
If you do decide to see your GP, you will most likely be referred to see a vascular specialist if your veins are causing a significant functional disturbance. If you have purely cosmetic concerns about the appearance of leg veins, it is highly unlikely that you will qualify for NHS treatment. Increasingly, even varicose veins that are causing functional issues and are causing significant symptoms, are also not being seen in the NHS due to a lack of funding.
Varicose Veins Treatment
Treatment for varicose veins is not always required, which is why the reduction in the provision of varicose vein treatment in the NHS is reduced. For patients who are not suffering from functional symptoms and are not concerned about the cosmetic appearance of leg veins, then there may be no need to have immediate treatment especially if they have not worsened over time.
RELATED: Best Treatments for Varicose Leg Veins
Having said that, the presence of varicose veins is confirmation of underlying valve dysfunction in the deep veins and the most effective treatment to address this and lower pressure in the legs is to have the correct treatment. That’s why we would always recommend in these cases to have treatment for varicose veins as the raised pressure in the veins can lead to changes in the overlying skin, such as venous eczema, and when this is allowed to progress, can sometimes result in a venous ulcer which is often painful and difficult to treat.
The traditional form of treatment for varicose veins is known as ligation and stripping, carried out by a vascular surgeon and most commonly requires a general anaesthetic and overnight stay. Surgical treatment for varicose veins has been almost completely superseded by more minimally invasive techniques such as EVLA. Adopting a minimally invasive approach to the treatment of varicose veins results in a lesser impact on the body compared with more invasive surgical approaches. The gold standard treatment for vein treatment, EVLA only requires tiny incisions and can be done under local anaesthetic and carries a very quick recovery with minimal risk of complications. At Centre for Surgery, we specialise in offering minimally invasive treatments for vein removal and are always aided by the use of colour duplex ultrasound medical imaging. The beginning of your patient journey starts with a comprehensive medical consultation to assess the condition of your leg veins and to pinpoint the precise underlying cause. With the identification of the underlying cause of prominent vein formation, an effective treatment plan can be formulated. The key to successful treatment is to locate and eradicate veins which are responsible for valve dysfunction before going on to address the prominent and unsightly leg veins under the skin surface. With effective treatment of the underlying causes of prominent leg veins, a significant reduction in symptoms can be expected, along with a marked improvement in the appearance of the leg with a much lesser chance of the problem recurring. Centre for Surgery takes great care to follow the latest national guidelines from the National Institute for Health and Care Excellence (NICE). NICE has issued clear guidelines that emphasise the importance of carrying out minimally invasive treatments, including EVLA and avoiding surgery where possible. Unfortunately, in many centres across the UK, the default approach for the treatment of varicose veins is a surgical ligation and stripping procedure, which is not in line with national guidance. In our experience, in the vast majority of cases, there is no need for a surgical approach to treat varicose veins.
After your doctor assesses you with a full medical history, physical examination and a duplex ultrasound assessment, the most appropriate treatment will be recommended based on the clinical imaging findings. For patients with a confirmed diagnosis of varicose veins, the best treatment is endovenous laser ablation (EVLA) as a first-line procedure followed by either foam sclerotherapy and/or vein avulsions, also known as phlebectomy as a second stage treatment. Patients who have thread veins or spider veins may benefit from microsclerotherapy injections or long-pulse Nd:YAG laser.
With traditional surgical treatment for varicose veins, the long saphenous vein, which is the most prominent superficial vein of the leg, is surgically tied off (ligation) before being removed (stripping). The stripping procedure is very traumatic, with a high risk of complications, including nerve injury and significant post-operative pain and discomfort. Our treatment approach is different, with an emphasis on treating the vein from within, also known as an endovascular treatment, with no requirement to physically remove the vein from the body. Better treatment outcomes are possible with treatment using only local anaesthetic and with a far lower risk of complications such as bleeding and infection. This means patients can return to their normal activities much quicker.
Published studies consistently demonstrate lower recurrence rates after EVLA and other minimally invasive techniques compared to surgery. Revision rates after having had surgery can be as high as 60 to 70%. Experts say recurrence rates after EVLA can be as low as 1.5%.
Minimally invasive techniques such as EVLA, foam sclerotherapy, vein avulsions and/or phlebectomy are definitive treatments for varicose veins. However, there are several simple measures patients can take to improve symptoms of having varicose veins, including:
- Avoid prolonged periods of standing up
- Exercise regularly
- When seated, keep your legs elevated
- Wearing appropriate medical-grade compression stockings
Should I undergo screening for prominent veins?
We would advise against screening any type of leg veins if you have no symptoms and you have not noticed any prominent veins. It is not uncommon for many clinics to offer screening services for leg veins. As an ethical medical practice, we believe this offers no significant benefit for the patient and often comes at a significant expense. Even in cases when a duplex ultrasound scan discovers a problem with the valves in the veins, it is still best to wait until one develops symptoms or begins to notice the development of either varicose veins or thread veins, which are causing a cosmetic nuisance.
Further reading on varicose veins removal
What are the best varicose vein treatments?
What are alternative treatments for varicose veins?
Varicose veins recovery
Comparing varicose veins with healthy veins
Choosing the best varicose vein clinic in London
The treatment of varicose veins
What Are The Best Treatments For Varicose Veins?
FAQs
-
What are the causes of varicose veins?Varicose veins are prominent enlarged veins that are most commonly found in the legs. In severe cases, they can be very unsightly with bulging and twisty veins protruding from the skin surface. Thread veins or spider veins are the most common types of prominent veins found on the legs and do not protrude from the skin surface. Superficial veins which are normally found under the skin surface can develop into either thread veins or varicose veins if blood flow is impaired which is most commonly due to valve dysfunction leading to stretching out of the vein walls.
-
How do varicose veins develop?Blood normally flows in one direction towards the heart in a normal vein. Most veins have internal valves to facilitate this one-way flow of blood by opening to facilitate blood flow followed by the closure to prevent the back flow of blood. Varicose veins develop when the internal valves found in veins fail to function correctly. This leads to blood accumulating in the vein with a subsequent increase in vein pressure and it is this increasing pressure which leads to bulging of the vein giving rise to the common appearance of varicose veins.
-
How to stop varicose veins?Stopping the development of varicose veins entirely can be challenging because factors like genetics and age play a role. However, you can take steps to prevent them from worsening or delay their onset:
Stay Active: Regular exercise, especially walking, helps improve leg and vein strength.
Elevate Your Legs: Raise your legs above heart level whenever you can.
Avoid Prolonged Sitting or Standing: Change positions frequently.
Maintain a Healthy Weight: Extra weight can increase vein pressure.
Wear Compression Stockings: They help improve circulation.
Avoid Tight Clothing and High Heels: They can restrict blood flow. -
What are the risk factors for developing varicose veins?There are a number of factors which make people more likely to develop varicose veins:
Hereditary factors - if members of your family have varicose veins then you are more likely to develop them
Pregnancy - the changes in hormonal status and an enlarging uterus lead to pressure exerted on the large veins in the body which increase the risk of developing varicose veins
Female gender - Women are more likely to develop varicose veins than men due to the influence of hormonal factors
Obesity - Patients with higher body mass index will have an increased propensity to develop varicose veins due to the extra weight placing strain on the veins
Age - As we get older the body begins to lose elasticity and this also occurs in veins which increases the likelihood of them stretching out and developing varicosities -
What are the symptoms of varicose veins?The symptoms of varicose veins can develop even without the obvious appearance of varicosities on the legs. Normal veins found in the legs can become either thread veins or varicose veins if blood flow is impaired and unable to flow properly through the veins. When the vein walls stretch and enlarge this leads to the appearance of varicose veins which often resemble bunches of grapes under the skin. Thread veins do not protrude upwards from the skin, unlike varicose veins. Leg veins become visible when valve failure develops either in the deep venous system or the superficial venous system of the legs.
Aching or a heavy sensation of the legs - Patients commonly complain of a heavy load affecting their legs which causes them to tire easily and this can sometimes be associated with pain on touching the lakes and associated leg swelling.
Cramping - As a result of valve failure, blood tends to pool in the veins and this can give rise to a throbbing sensation in the legs which is often worse towards the end of the day
Itchiness - Although many patients may have dry skin on the legs, many patients develop characteristic flakiness or itching of the skin of the lower legs when varicose veins are present
Swollen ankles - As a result of the pooling of blood in the lower legs it is more common to experience swelling affecting the legs and ankles in those who have varicose veins
As well as being a cause of the symptoms listed above, varicose veins are also a significant cosmetic nuisance and often lead many people to cover up their legs when in public. The best approach is to see a vein specialist at Centre for Surgery for faster diagnosis and effective treatment. -
Do varicose veins develop in other areas of the body?The development of prominent and unsightly veins not only occurs in the legs but in a number of other areas including the scrotum where they are medically referred to as a varicocele also known as its older description of a "bag of worms". Varicocoele formation should always be thoroughly investigated to rule out underlying causes. Women can also develop a similar condition which is a recognised cause of chronic pelvic pain as well as the formation of prominent unsightly veins on the external genitalia. Both of these medical conditions can be effectively treated with an interventional radiology technique known as embolisation.
At Centre for Surgery, our practice is devoted exclusively to the treatment of leg veins including both varicose veins and thread veins. -
What are the home remedies for varicose veins?Witch Hazel: Applying this can reduce pain and swelling.
Apple Cider Vinegar: Some people believe massaging this onto varicose veins improves circulation, though scientific backing is limited.
Horse Chestnut Seeds: Available in capsule form or as a gel, these might reduce symptoms, but consult with a doctor before use.
Grape Seed Extract: Thought to improve blood circulation and reduce swelling.
Elevate Your Legs: Helps reduce swelling and improve blood flow.
Cold Water: Splashing cold water on your varicose veins can help reduce swelling and the sensation of heaviness. -
Is varicose vein treatment available on the NHS?It is increasingly more difficult to get treatment for varicose veins on the NHS due to funding pressures. Only the most severe cases with significant impairment of normal activities may qualify for treatment. In the first instance, you may be recommended non-surgical treatments such as compression stockings for symptom relief. Those who have varicose veins and are primarily causing a cosmetic nuisance will not be eligible for treatment in the NHS and you will be recommended to have treatment at a private clinic.
-
What are the risks of not having varicose veins treated?Pain: They can become achy and uncomfortable.
Swelling: The area around varicose veins may swell.
Skin Changes: Over time, the skin near varicose veins can become discoloured or dry.
Ulcers: Painful ulcers can form on the skin near varicose veins, especially near the ankles.
Blood Clots: Veins deep within the legs can swell, a condition called thrombophlebitis.
Bleeding: Veins very close to the skin may burst. -
Will my varicose veins get worse?Varicose veins tend to be a progressive condition, meaning they can get worse over time if not treated. Factors like genetics, pregnancy, age, and prolonged standing can contribute to their progression. Following preventive measures can help delay their progression, but they may not stop it entirely.




